-
Background
A 44-year-old male presented at a local orthopedic office with right knee pain and swelling. The patient reported he had initially injured his knee in 2014 while playing basketball, at which time he jumped and upon landing, twisted the knee. After several weeks of rest to allow for the swelling and pain to subside, the patient attempted to return to playing basketball; however, his symptoms continued to worsen.
The patient initially underwent a medial meniscus repair and chondroplasty followed by a subsequent meniscectomy while under the physician’s care. Following these procedures, the patient was still unable to play basketball and stated that running had become painful. As a result, the patient obtained a second opinion, at which time he was diagnosed with a loose body and treated via surgical removal of the fragment. This intervention was also ineffective in relieving the patient’s knee pain. A third physician was then consulted, who administered an injection of hyaluronic acid (HA) into the patient’s knee. This injection provided the patient with some benefit and relief but the pain soon returned. After over one and a half years of unsuccessful treatment and continued pain, the patient was referred by the third physician to Pacific Regenerative and Interventional Sports Medicine (PRISM).
-
The Case
The patient presented at PRISM experiencing pain of the right anterior knee that was deep within the joint. In addition, the patient noted medial pain, occasional “locking”, and pain when descending steps or squatting. Given these complaints, the patient was examined for suspected knee pathology.
Upon physical examination, the patient was found to have a mild effusion. He displayed tenderness upon palpation along the medial joint line, at the insertion of the quadriceps tendon and along the lateral joint line. A bony defect was palpated at the tibial insertion of the patellar tendon. Patellar Compression test and McMurray’s test were positive. After examination, the patient’s recent MRI studies were analyzed for pathology.
The patient’s MRI revealed a blunting of the patient’s medial meniscus with a suspected radial tear, as well as a possible tear of the lateral meniscus. In addition, a significant cartilage defect of the medial femoral condyle, a chondral defect in the trochlea and thinning of the cartilage in the patella, adjacent to the trochlear defect were also evident. Based on the physical exam and MRI, treatment options were discussed including an allograft osteoarticular transfer system (OATS) and biologic scaffolding for cartilage restoration of the trochlea and the femoral condyle. Given the patient’s age and activity level, an attempt at cartilage restoration was determined to be the best option.
The Answer
The patient underwent the cartilage restoration procedure and was evaluated six months post-surgery using an in-office arthroscopy (mi-eye 2) to assess the healing of the procedure. The patient had experienced some pain and swelling prior to the mi-eye 2 procedure, which required aspiration prior to the procedure. Once fluid was removed, the patient was prepared for the in-office arthroscopy.
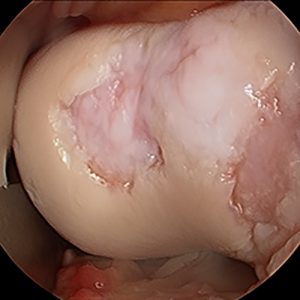
The mi-eye 2 procedure was performed using a standard sterile technique. Both the anteromedial and anterolateral portals of the knee were prepared using a ChloraPrep scrub. Local anesthesia was obtained through utilizing 5cc of 1% lidocaine in each portal. The scope was first introduced into the patellofemoral space to evaluate the graft, which appeared to be well-established with mild chondromalacia. The scope was then introduced into the lateral joint space, revealing a good fill of the surgically restored cartilage area and again only mild chondromalacia. Finally, the scope was introduced to the medial aspect of the joint where mild chondromalacia was revealed.
Upon completion of the in-office arthroscopy, the mi-eye 2 scope was removed and discarded in a sharps bin. The knee was cleaned to remove remaining fluid and Steri-Strips were applied to the all portals. The patient was given a compression sleeve to be worn for the remainder of the day. Overall, the patient tolerated the mi-eye procedure without any complications and was discharged in good condition.
Discussion
This previously very active patient was almost completely sidelined from all athletic and recreational activities secondary to his knee pain. He was found to have numerous significant cartilage lesions in various areas of the knee. Resurfacing of his cartilage was only the first step to his recovery. The patient and surgeon had to be confident that the appropriate healing had occurred so recreational clearance could be achieved. The use of the mi-eye 2 in-office arthroscopy allowed for direct visualization of the patient’s successful cartilage restoration. Historically, a second arthroscopy in the operating room may have been required to achieve this visualization.
When presented with the options, the patient opted for the in-office procedure, which provided an immediate answer for both the patient and physician. In addition, the use of mi-eye 2 saved the patient an additional trip to the operating room and the cost, anesthesia event and recovery associated with the surgery. Clinically, the mi-eye 2 displayed clear visualization of the previous cartilage procedure and confirmed healing of the surgically restored areas.