-
Background
The patient, a 22-year-old female student/office worker, originally presented in the office with right knee pain that she had been experiencing for several years. The patient stated that she was very active, participating in a variety of activities ranging from running and sports to general physical fitness. Her knee pain had impeded her ability to maintain this lifestyle at the desired level.
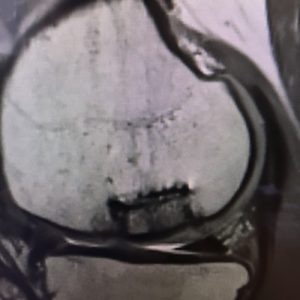
After a physical examination, it was decided that additional imaging studies were needed to fully understand the cause of her pain and injury extent. She proceeded to have an x-ray, computerized tomography (CT) scan and magnetic resonance imaging (MRI) performed. The studies found that the patient had osteochondritis dissecans (OCD) which was affecting the medial femoral condyle of her right knee. At that time, she was scheduled for arthroscopic fixation of the OCD.
Following the initial OCD procedure, the patient did not experience any pain relief in her knee. A second intervention in the form of an open, osteoarticular transfer system (OATS) procedure was then performed. Just as with the patient’s first procedure, this did not show any signs of healing or offer the patient pain relief. After a discussion with the patient about her options, it was decided to have a third intervention involving bone grafting and drilling the site to promote revascularization and reossification.
-
The Case
The third surgical intervention resulted in the patient being relieved of her knee pain for approximately six months, post-operatively. She then returned at seven months following surgery with renewed knee pain. In addition, the patient was experiencing a catching and popping sensation in the joint. Upon examination, it was found that the patient had a high level of tenderness in the area of the medial femoral condyle. The tenderness was located in the same area in which the surgical interventions had previously been performed, which raised concern regarding the previous procedure.
Based on the findings of the examination, in conjunction with her surgical history, we discussed the patient’s options, including an in-office arthroscopy via the mi-eye 2™ scope to assess the effectiveness of the previous procedure and the state of the articular cartilage and bone graft. Ultimately, the patient opted for the in-office arthroscopy, which was then performed the same day in the office.
The Answer
The mi-eye 2™ in-office procedure was performed using a standard, sterile technique. The patient was positioned seated on the edge of examination table with her right knee suspended, creating approximately 90 degrees of flexion. The skin around the portal location was then aseptically prepared using betadine. Local anesthesia was attained via 10cc of 1% lidocaine injected into the dermal area around the portal and subcutaneous
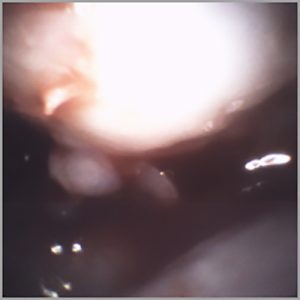
tissue down to the capsule. Adequate time was then given for the lidocaine to take effect, at which time the patient’s skin was re-prepared and the mi-eye 2™ was introduced to the joint.Upon entry into the patient’s medial compartment, the mi-eye 2™ visualized the femoral condyle and the site of the surgical intervention. The prior drilling and bone grafting were found to be intact and in good condition. There was also
evidence that healing was occurring along the confluence of the graft and articular cartilage. With further examination, it was discovered that the patient had evidence of degeneration occurring in the cartilage adjacent to the bone graft. In addition, a cartilage flap and loose body was found, which may be the cause of the patient’s pain. Prior to procedure completion, a corticosteroid injection was administered via the integrated luer port of the mi-eye 2™ to aid in the patient’s pain.Following the injection, the mi-eye 2™ was removed and the portal was covered with a bandage. During the procedure, the patient was able to observe and understand the condition of her knee. She experienced no pain from the procedure and only felt slight pressure while the scope was in her knee.
Discussion
The mi-eye 2™ was instrumental in the case of this patient as it allowed for visualization and inspection of the patient’s previous surgical intervention. Using the mi-eye 2™, it was confirmed that the cartilage overlying the graft had survived and incorporate with the native tissue. In addition, the mi-eye 2™ allowed for direct visualization of degenerative changes, a cartilage flap and loose body in the adjacent cartilage. Direct visualization allowed us to view these new pathologies, which will allow for diagnosing whether they are the cause of the recurring knee pain, and whether they require any treatment. Following the findings, the patient was sent for a follow-up testing to assess if the bone graft is still stable and whether it has incorporated into the patient’s native bone.
The mi-eye 2™ gave the capability to investigate and assess the patient’s knee without the need to return to the operating room, rather completing the assessment in the office. With the patient only under local anesthesia, she was also able to watch as the procedure was occurring. As a result, this allowed for a dynamic and real-time explanation of the patient’s condition. In addition, the discovery of pathology during the procedure with the patient present allowed for an immediate discussion into next steps. As such, in this case, the mi-eye 2™ may help in accelerating the timeline for pain resolution