-
Background
The patient, a 26-year-old, male, professional tennis player, presented with a one-year history of increasing shoulder pain that limited his ability to play tennis. Hitting serves and overheads were particularly painful and led to his inability to compete on the professional tennis tour. Of note, 2 years prior, the patient had undergone an arthroscopic SLAP repair by a surgeon in South Korea. His exam was consistent with labral pathology and an MRI showed a small tear of the anterior labrum. He was prescribed a course of formal physical therapy, which helped improve his range of motion including internal rotation and his rotator cuff strength; however, the patient continued to have a positive Active Compression Test, positive overhead valgus stress test and pain with apprehension.
-
The Case
Given the patient’s failure to return to competitive tennis with rest and physical therapy, we then discussed the potential benefits of various injections compared to surgical intervention. Taking into account the patient’s age and that he had previously missed several seasons due to shoulder pain and surgery, it was felt that another surgical procedure and subsequent rehabilitation would likely result in the end of his professional tennis career. As a result, the treatment discussion shifted towards the benefits of an intra-articular injection of platelet-rich plasma (PRP) or cortisone injection as a way to treat his shoulder pain. After discussing the risks and benefits with the patient, it was decided to proceed with a PRP injection. Traditionally, the injection is administered into the intra-articular space with the assistance of fluoroscopy or ultrasound guidance. In this specific case, a new option was utilized via the mi-eye 2™, an in-office diagnostic scope, which would provide direct visualization of the injection for precise placement.
The Answer
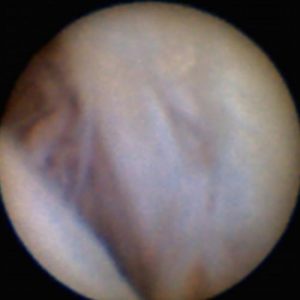
The mi-eye 2™ diagnostic arthroscopy procedure was performed in the physician’s office setting. The patient was positioned with the shoulder facing outwards, allowing for optimal access from the posterior aspect of the joint. A standard, aseptic technique was utilized to prepare the site and the shoulder was draped. The posterior portal to the glenohumeral joint was injected with 10cc lidocaine—4cc in the dermal area and the remaining 6cc in the joint. The patient was left for ten minutes to allow the lidocaine to take effect and numb the patient’s shoulder. The mi-eye 2™ was then introduced into the shoulder joint following the same path as the previous injection. A syringe containing sterile saline was attached to the luer port to assist in clearing the visualization. Upon entering the joint, the camera inside the needle was exposed enabling the visualization. The mi-eye 2™ quickly confirmed the suspected tear of the anterior labrum.
Under direct visualization of the labral pathology, PRP was then injected directly into the site of the tear through the integrated luer port on the mi-eye 2™ probe. When the PRP injection was completed, the mi-eye 2™ was removed from the shoulder, disposed of in the sharp’s bin and the portal site was covered with a standard bandage.
Throughout the mi-eye 2™ procedure, the patient experienced little to no pain. The patient was prescribed a new round of physical therapy after the PRP injection. At six weeks following the procedure, the patient returned to being able to hit tennis balls without shoulder pain. Three months after the mi-eye 2™ procedure and PRP injection, the patient was able to return to competitive tennis.
Discussion
Traditionally, injections such as PRP required the use of indirect visualization via fluoroscopy or ultrasound. The use of the mi-eye 2™ scope allowed for precision in the placement of the injection through the technology’s direct visualization of the patient’s pathology. While fluoroscopic and ultrasound guidance is an effective mode of placement for PRP injections, the mi-eye 2™ offers a new alternative that allows a physician to view the pathology, leading to a higher certainty and confidence in the effective placement of injected material.